Team Develops New Tagging Technique for Better Cancer Detection
Research shows a promising new avenue for early tumor detection
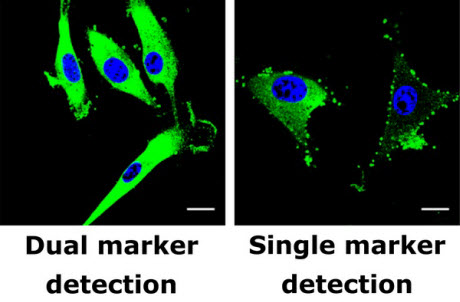 Weibo Cai and colleagues at the University of Wisconsin-Madison have developed a technique that detects a pair of markers for glioblastoma, a type of brain cancer. Left: Cancerous cell is marked with green (blue shows cell nucleus but does not indicate cancer). Right: When only one marker, called epidermal growth factor receptor, is detected in the same sample, the cancer signal is much less obvious.Image Credit: Weibo Cai lab, University of Wisconsin-MadisonTagging a pair of markers found almost exclusively on a common brain cancer yields a cancer signal that is both more obvious and more specific to cancer, according to a study published last week in the Proceedings of the National Academy of Sciences (PNAS).
Weibo Cai and colleagues at the University of Wisconsin-Madison have developed a technique that detects a pair of markers for glioblastoma, a type of brain cancer. Left: Cancerous cell is marked with green (blue shows cell nucleus but does not indicate cancer). Right: When only one marker, called epidermal growth factor receptor, is detected in the same sample, the cancer signal is much less obvious.Image Credit: Weibo Cai lab, University of Wisconsin-MadisonTagging a pair of markers found almost exclusively on a common brain cancer yields a cancer signal that is both more obvious and more specific to cancer, according to a study published last week in the Proceedings of the National Academy of Sciences (PNAS).
The research, from the University of Wisconsin-Madison, shows a promising new avenue for early tumor detection that, in principle, should apply to a wide range of cancers. The new technique also suggests methods for more precise cancer treatment.
The idea of searching for two markers has been around for a while, but it was technically very difficult to achieve, says co-first author Haiming Luo, a UW-Madison postdoctoral researcher in the Department of Radiology.
 Weibo CaiPhoto courtesy of the University of Wisconsin-MadisonThe researchers were directed by Weibo Cai, an associate professor of radiology and medical physics in the UW School of Medicine and Public Health. They created antibodies that are specific to two proteins that often mark brain tumors. One marker, called CD105, appears on new blood vessels, which in adult humans only grow during pregnancy or when wounds heal. Mutations in the other marker, epidermal growth factor receptor, spark uncontrolled cell division in a number of cancers, including glioblastoma.
Weibo CaiPhoto courtesy of the University of Wisconsin-MadisonThe researchers were directed by Weibo Cai, an associate professor of radiology and medical physics in the UW School of Medicine and Public Health. They created antibodies that are specific to two proteins that often mark brain tumors. One marker, called CD105, appears on new blood vessels, which in adult humans only grow during pregnancy or when wounds heal. Mutations in the other marker, epidermal growth factor receptor, spark uncontrolled cell division in a number of cancers, including glioblastoma.
To make a structure able to bind to both of these markers, the researchers chopped off unneeded sections of each antibody, then assembled them with a fast, reliable joint. The construct contained a fast-decaying isotope that can be detected in a PET (positron emission tomography) scanner.
After purifying the detection compound to remove unpaired antibodies, the researchers injected the remainder into mice that had received transplants of human glioblastoma tumors.
After waiting up to 36 hours for the detector molecules to link to tumors or clear from normal tissue, the researchers searched with a PET scanner for the radiation they released. The result was a great increase in the intensity of the signal, compared to conventional PET scanning.
A second benefit was specificity: The detector linked to tumors, yet hardly any connected to healthy tissue.
When PET scans are used to detect cancer, they usually look for glucose metabolism — a sign of biological activity that can be linked to cancer, or many other possible causes. Activity in the brain, where cancer detection is particularly troublesome, can mask the signal of cancer.
The study points toward a "toolkit" approach to cancer detection, says co-first author Reinier Hernandez, a graduate student in medical physics. Studies on other tumors are progressing, he says, based on well-known targets on particular cancers that appear in genetic databases.
By demonstrating a new way to connect to tumor cells while avoiding normal tissue, the new technique immediately suggests ways to treat cancer rather than just identifying it, Hernandez says. "The whole field is moving toward more specific treatment, rather than chemotherapy, which can damage healthy tissue as well as tumors."
The two-part antibody could, for example, be joined to a strong, quick-acting unit of radiation, or to a chemical that can kill cells, says Cai.
Finally, the detector could be used to assess the progress of treatment — a growing need now that so many new possible cancer treatments are under study.
"As we learn more about cancer and what distinguishes it from healthy tissue," Cai says, "we are able to bring to bear our expanding ability to detect and manipulate genes, proteins and other molecules, both for detection and for therapy."
