Improving Clinical Specimen Management
Across health care and drug development, experts need advanced tools to manage specimens and their associated data
 Brain tissue can be one of the most difficult samples to collect.Image courtesy of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health
Brain tissue can be one of the most difficult samples to collect.Image courtesy of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health
Finding a specific sample at any time remains challenging
On July 4, 2016, ClinicalTrials.gov listed 62,931 open clinical trials. Running and analyzing those trials requires companies to manage a staggering number of specimens. “There’s a broad global supply chain for a clinical trial specimen,” says Michael Brookman, chief information officer for Q2 Solutions (Morrisville, NC), a global clinical trials laboratory services organization that is a joint venture between Quintiles (Durham, NC) and Quest Diagnostics (Madison, NJ). “It starts with the setup of the protocol, and then a kit is put together based on the specific testing that has to be done,” Brookman explains. “After that, the kit leaves the central lab provider, and both the sponsor and the central lab lose sight of where it travels until it comes back.”
As a clinical trial kit makes its journey, specimens may go to three or four places—some to a clinical trial site for local testing; others to hospitals; and some to third parties, like labs or biorepositories. “There’s not great visibility in the supply chain,” Brookman says, “and it’s not always clear how that impacts the patients or the sponsor.”
Other experts also see much room for improvement in today’s specimen procurement and management processes. Christopher Ianelli, chief executive officer of iSpecimen (Lexington, MA), points out a well-known problem that starts in preclinical research and goes through to clinical trials: a dearth of high-quality, data-rich human biospecimens. He adds, “Particularly with the surge of personalized medicine research, qualified human samples— with very specific specimen- and patient-level criteria— are in tremendous demand.” Nonetheless, Ianelli believes that traditional identification and procurement methods fail to produce “the right samples from the right patients.” As he notes, “One National Cancer Institute study found that 81 percent of researchers reported limiting the scope of their work due to a shortage of both quality and quantity of biospecimens.”
Across health care and drug development, experts need advanced tools to manage specimens and their associated data.
Getting More
In many cases, the steps in a clinical trial’s supply chain are not well-known. “Maybe three or four steps out of ten take most of the processing time, but you don’t understand that,” Brookman says. To make a clinical trial more efficient and effective, the sponsor and the people running a trial need to know how the chain of steps really works.
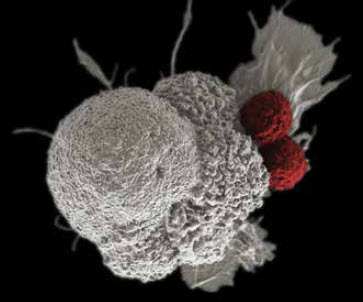 Immunotherapy could battle many kinds of cancer, as shown here by cytotoxic T cells (red) attacking an oral squamous cancer cell (white), and improved specimen management can provide more samples to study.Image courtesy of Rita Elena Serda, Duncan Comprehensive Cancer Center at Baylor College of Medicine, National Cancer Institute, National Institutes of Health.The people analyzing the results also need to be sure that everyone involved followed the protocol. “Did they collect the right sample, do the right processing steps when collecting it, and ship it under the correct conditions,” Brookman asks. If these things aren’t done correctly, a clinical trial cannot produce accurate results.
Immunotherapy could battle many kinds of cancer, as shown here by cytotoxic T cells (red) attacking an oral squamous cancer cell (white), and improved specimen management can provide more samples to study.Image courtesy of Rita Elena Serda, Duncan Comprehensive Cancer Center at Baylor College of Medicine, National Cancer Institute, National Institutes of Health.The people analyzing the results also need to be sure that everyone involved followed the protocol. “Did they collect the right sample, do the right processing steps when collecting it, and ship it under the correct conditions,” Brookman asks. If these things aren’t done correctly, a clinical trial cannot produce accurate results.
The turnaround time for the data also impacts efficiency and inclusion criteria to quickly enroll patients. “Some steps might not need to take as long as they do,” Brookman explains.
The data also need to be readily available throughout the process, especially as the industry talks of adaptive clinical trials. In an adaptive trial, the team can change the protocol during the process. This can help the sponsor adjust, for example, the targeted patient population, such as patients with a specific gene or genetic mutation. To do that, though, people running a trial need specific information about every specimen. “You need that down to the tube level,” Brookman explains.
In summary, someone designing a clinical trial needs to answer three questions. First, how do you measure the supply chain? Second, how do you get data faster? And third, how do you enable adaptive trial design? The answer to all three questions is advanced specimen-management technology.
A Tech Trio
Brookman thinks of the necessary technology in three buckets: core technology, sample tracking, and the Internet of Things (IoT).
For core technology, he means in-house applications, including the protocol-management systems. Technology is already available to manage the protocol and specimens.
To keep track of the samples as they travel through the supply chain, trial sponsors face some challenges. You’d like consent attached to every vial. That is, you want to know what the patient has agreed can and cannot be done with that sample, and to know that and the location and status of every vial throughout the trial. “Mobile devices and different tracking technologies can provide two-way dialog— readable and writable—to every vial,” Brookman says, “but this technology is primarily in a beta, or pilot, mode.”
The IoT technologies lie further ahead. “This would put devices at an investigator’s site and transmit back data to the provider—like Q2 Solutions or the sponsor—to get information about specimens in closer to real time,” Brookman says, “and this is more in an alpha mode.”
To realize this trio of technologies, clinical trial sponsors and participants must wait—at least to get the complete package.
The Right Start
The success of managing samples starts with obtaining them, and some take more care than others do. Biospecimens come in many classes, including biofluids—blood, saliva, serum, etc.—and tissues, which are more difficult to obtain. Alexander Vortmeyer, a visiting professor at Indianapolis University and an expert in tissue procurement, says that brain tissue is the most difficult sample to collect.
He points out three main challenges. First, he says, “Obtaining tissues from brain tumor resection does not mean you received any tumor at all.” Second, he notes, “Even if you are sure you received tumor, it may not be representative for the final diagnosis.” And third, Vortmeyer points out, “Even if you received representative tumor, you do not know whether it is viable.”
In the face of those challenges, Vortmeyer says, “The only way to overcome those challenges is through awareness, competence, and extra effort.” He adds, “Pathology input may enable performance of additional procurement strategies that would allow for better differentiation of the tissue specimen with potential analysis of different tissue components—for example, diseased versus non-diseased tissue components.”
Cloud Collections
iSpecimen has developed advanced technology to manage the identification and procurement of clinical specimens, including biofluids, solid tissue, and cells, as well as the delivery of real-time data. As Ianelli explains: “Our cloud-based technology interfaces with data systems, including electronic medical records and laboratory information systems, throughout our diverse partner network of hospitals, labs, biorepositories, blood centers, and other healthcare organizations with access to human specimens.”
Specimen tracking makes up a crucial part of this process. “Through this technology,” Ianelli says, “we are able to watch patient and specimen flow at our partner organizations, along with the highly valuable specimenand patient-level data associated with them.”
iSpecimen’s technology allows research customers to request specimens based on important inclusion and exclusion criteria to meet their study needs, including specimen type, disease state, patient demographics, past medications and treatments, and molecular or genomic data. When a sample and its data annotation meet a customer’s criteria, iSpecimen’s technology manages the pickup, packing, and shipment processes of the specimens and electronic delivery of the data.
Benefits of scale also come into play. Ianelli says that its partner sites see tens of millions of samples a year. “The diversity of specimen types that we see by aggregating supply sites throughout the country to create our partner network enables us to source traditionally difficult-to-find orders,” he says. As an example, he described the interest in checkpoint inhibitors as immunotherapeutics for cancer, but the U.S. Food and Drug Administration has only approved three medicines in this class. To develop more checkpoint inhibitor-based treatments, researchers need more patients to study. “Just recently, we were able to fulfill an order for matched sets of specimens from lung cancer patients with a history of checkpoint-inhibitor treatment,” Ianelli says. “These sets included frozen cancerous tissue, normal adjacent tissue, plasma, and viable peripheral blood mononuclear cells.”
In The Clinic
 The University of Rochester Medical Center lab handles about 12,000 samples every day, and that requires advanced specimen management.Image courtesy of Bethany Bushen, marketing manager, UR Medicine Labs, University of Rochester Medical CenterSimilar challenges exist for specimens being used to treat a patient. When asked about the key challenges in managing clinical specimens, Melissa Allen, pre-analytical operations manager at the University of Rochester Medical Center (NY), mentions several, including errors made in collecting a sample. “These errors include specimen identification errors and collection errors—wrong tube, wrong order of draw, poor technique, and contamination,” she says.
The University of Rochester Medical Center lab handles about 12,000 samples every day, and that requires advanced specimen management.Image courtesy of Bethany Bushen, marketing manager, UR Medicine Labs, University of Rochester Medical CenterSimilar challenges exist for specimens being used to treat a patient. When asked about the key challenges in managing clinical specimens, Melissa Allen, pre-analytical operations manager at the University of Rochester Medical Center (NY), mentions several, including errors made in collecting a sample. “These errors include specimen identification errors and collection errors—wrong tube, wrong order of draw, poor technique, and contamination,” she says.
Once a sample gets collected, keeping track of it poses another challenge. For example, Allen says that loss of specimens due to the logistics of moving specimens around their system is another challenge. “Our lab moves about 12,000 specimens through its system daily,” she explains. “We have over 1,000 pickup stops per day delivering specimens to both our main hospital-based laboratory and our off-site outpatient laboratory location.”
To take on these challenges, Allen’s group uses electronic medical record software from Epic (Verona, WI) with computerized physician order entry and interfaced to a laboratory information system. Allen says, “This has significantly reduced, but not eliminated, order entry and identification issues.” They also use courier tracking software. “The use of barcoded specimen bags, handheld scanners, and GPS tracking software give us real-time information on the locations of our drivers and our specimens,” Allen explains.
Keeping track of patient samples poses a challenge for everyone in health care. When asked about the key challenges in managing patient samples, Dede Haverstick, director of clinical chemistry, specimen management, and referral testing services at the University of Virginia, says, “For blood tubes and urine specimens, it is finding the sample in the lab—physically—for add-ons and/or repeat testing if results are questioned by the ordering physician.” To do that, says Haverstick, “We have an in-house barcode-linked specimen retrieval system, but will be installing the Abbott ACCELERATOR line with tube storage within the next five months.”
So from treating patients today to developing medicines for tomorrow, managing the specimens lies at the heart of successful medicine.
