Mastering aseptic technique is a cornerstone skill for any professional working in a biological laboratory, particularly those engaged in cell culture. This comprehensive guide will equip you with the knowledge and actionable protocols needed to prevent contamination, improve the reproducibility of your experiments, and achieve consistent, high-quality results. We'll dive into the fundamental principles, essential equipment, step-by-step procedures, and common pitfalls, all with the goal of helping you elevate your practice and protect your valuable research.
Understanding the Principles: Aseptic vs. Sterile
ImageFX (2025)
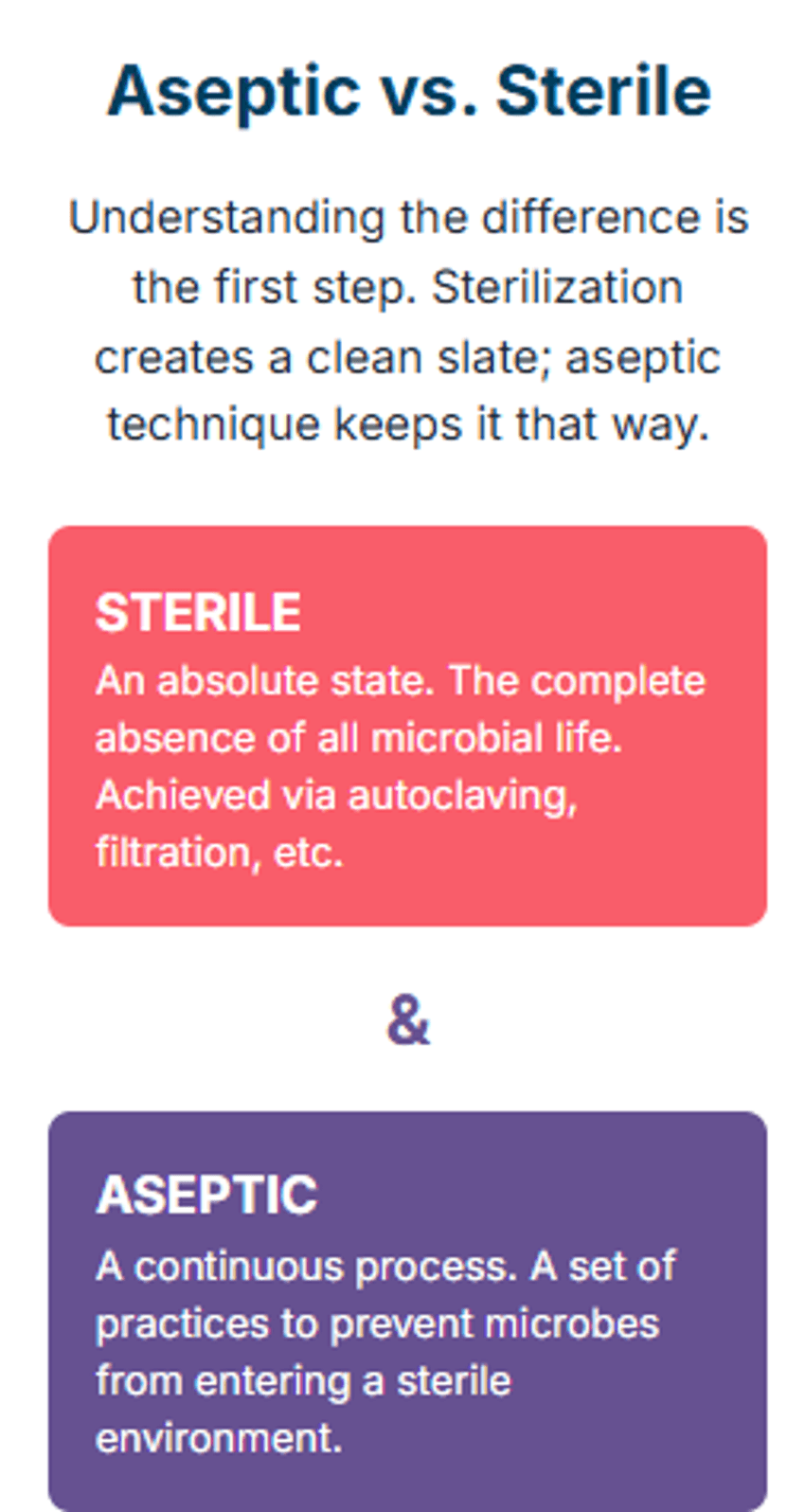
Before we delve into the specifics of aseptic technique, it's crucial to understand the distinction between asepsis and sterility. While often used interchangeably, these terms represent different but complementary concepts in a laboratory setting.
Sterilization is a process that destroys or eliminates all forms of microbial life, including bacteria, viruses, fungi, and spores. This is an absolute state. An item is either sterile or it is not. Examples of sterilization methods include autoclaving, dry heat, filtration, and chemical agents. The goal is to create a starting environment that is completely free of microorganisms.
Aseptic technique, on the other hand, refers to the set of practices and procedures performed under controlled conditions to prevent contamination from microorganisms. It's not about achieving an absolute absence of life, but rather about meticulously preventing unwanted organisms from entering and proliferating in a sterile environment or sample. Think of it as a continuous process of maintaining a sterile field. In cell culture, you begin with sterile media, sterile vessels, and sterile cells, and your aseptic technique is the skill set you use to handle these components without introducing contaminants from the surrounding air, surfaces, or even yourself. The difference is subtle but vital: sterilization creates the contamination-free zone, while aseptic technique maintains it.
Essential Equipment and Workspace Management for Aseptic Procedures
Your success with aseptic technique is directly linked to the proper use and maintenance of your equipment and workspace. The primary tool for any cell culture work is the biosafety cabinet, or laminar flow hood.
A BSC creates a sterile working environment by continuously filtering air through a HEPA (High-Efficiency Particulate Air) filter, providing a constant flow of sterile air over the work surface. The key to using a BSC effectively is to understand its airflow dynamics.
- Proper Setup: Always turn on the BSC for at least 15 minutes before beginning your work to allow the airflow to stabilize and the work surface to be fully purged.
- Workflow: Arrange all necessary materials before you begin work and place them strategically within the hood. Keep all items at least six inches from the front grille to avoid disrupting the airflow and ensure the sterile air effectively bathes your workspace. Never block the rear air intake grille.
- Disinfection: Before and after each session, the interior surfaces of the BSC (side walls, back panel, work surface) must be thoroughly wiped down with a 70% ethanol solution. This simple step is a critical component of effective aseptic technique.
Personal Protective Equipment (PPE)
Wearing the correct PPE is non-negotiable for both personal safety and for protecting your cultures.
- Lab Coat: A clean lab coat should be worn at all times to prevent contamination from street clothes.
- Gloves: Sterile gloves are essential. Change them frequently, especially after touching non-sterile surfaces (e.g., door handles, pens) or if they become torn.
- Safety Glasses: Protect your eyes from chemical splashes and accidental aerosolized particles.
Essential Materials for Aseptic Work
A well-prepared workspace includes these essential items:
- 70% Ethanol: The gold standard for surface disinfection.
- Bunsen Burner or Alcohol Lamp: Used for flaming the mouths of bottles and pipettes to create a convection current of sterile air, further protecting against airborne contaminants.
- Pipettes and Tips: Use only sterile, disposable pipettes and tips.
- Sterile Media, Reagents, and Culture Vessels: All materials entering the BSC must be sterile.
Step-by-Step Protocol: Executing Aseptic Technique with Precision
Executing aseptic technique with precision is a skill honed through practice and vigilance. Here is a general protocol for handling cell cultures.
Preparation is Key: Before entering the cell culture room, tie back long hair, and remove any jewelry. Put on your clean lab coat, gloves, and safety glasses.
Disinfect the Hood: Spray the BSC's interior with 70% ethanol and wipe it down with a sterile lint-free wipe. Allow the alcohol to evaporate completely.
Gather Materials: Organize all media, reagents, and culture vessels neatly inside the hood, well within the designated work zone. Do not overcrowd the space.
Initiate the Procedure:
- Flame the necks of bottles and flasks before opening them and again before closing them. This action creates an upward convection current that prevents airborne particles from falling into the vessel.
- When pipetting, never let the non-sterile end of the pipette touch anything. Work over the work surface of the hood, not over other materials or bottles.
- Keep lids and caps facing downwards on the clean work surface to prevent dust or airborne microbes from settling on the inner, sterile side.
- Minimize the time that bottles, flasks, and plates are open to the air.
Final Cleanup: Once your work is complete, discard all used materials in the appropriate waste containers. Disinfect the hood surfaces again with 70% ethanol to ensure it is clean for the next user.
Common Contamination Sources and Troubleshooting Your Aseptic Process
Even with the best intentions, contamination can occur. Knowing the signs and sources is the first step to successful troubleshooting and improving your aseptic technique.
- Bacterial Contamination: Often appears as small, discrete, floating particles or a cloudy turbidity in the culture medium. Bacteria typically grow quickly, often making the medium appear murky within 24–48 hours. Under a microscope, they can be seen as tiny, shimmering specks.
- Fungal Contamination: Fungi, including yeast and mold, are common contaminants. Mold may be visible to the naked eye as fuzzy, off-white, or black growth on the surface of the medium. Yeast often appears as small, refractile spheres that do not adhere to the culture vessel and can be confused with dead cells.
- Mycoplasma Contamination: This is the most insidious form of contamination. Mycoplasma are tiny bacteria that lack a cell wall, making them resistant to many antibiotics. They do not cause visible turbidity and often go undetected, subtly affecting cell growth and experimental results. Regular testing is the only way to detect mycoplasma.
If you suspect contamination, immediately quarantine the culture and any materials used with it. Review your entire procedure, from handwashing to workspace setup, to identify any potential breaches in your aseptic technique. Consider whether any new reagents or shared equipment could be a source.
Best Practices for Maintaining a Contamination-Free Culture
The best defense against contamination is a proactive, disciplined approach to your work.
- Dedicated Workspace: Whenever possible, use a dedicated room or area solely for cell culture to minimize the risk of cross-contamination from other lab activities.
- Minimize Movement: Avoid unnecessary movements of your hands and arms inside the BSC, as this can disrupt the laminar airflow. Keep conversations and sudden movements to a minimum.
- Use Fresh Reagents: Always use sterile, fresh reagents. Avoid using a single large stock of media or supplements for a prolonged period. Instead, aliquot reagents into smaller, single-use volumes to minimize repeated exposure to air and potential contaminants.
- Training and Audits: Regularly review and practice your aseptic technique protocols. New personnel should receive extensive training and their work should be audited periodically to ensure best practices are being followed.
The Lasting Impact of Meticulous Aseptic Technique
In the world of cell culture, a single lapse in aseptic technique can jeopardize weeks or months of work. The time, resources, and valuable research data lost to contamination are a heavy price to pay. By mastering the principles outlined in this guide—understanding the difference between asepsis and sterility, preparing your workspace meticulously, and executing each step of your protocol with precision—you build a foundation for success. This isn't just about following rules; it's about developing a deep understanding of microbial risk and a disciplined approach to mitigating it. The result is more robust data, reproducible experiments, and a cleaner, more efficient lab environment, ultimately accelerating the pace of scientific discovery.
FAQ
What is the most critical step of aseptic technique for cell culture?
While all steps are important, the most critical element is the consistent use of the biosafety cabinet and the meticulous disinfection of all surfaces and materials before starting work. This establishes and maintains the sterile field.
How do I know if my cell culture is contaminated?
A: Visible signs include a cloudy or turbid appearance of the medium (bacteria), fuzzy spots or growth on the surface (fungi), or an unusual change in medium pH. For insidious contaminants like mycoplasma, regular testing is required.
Is it necessary to flame the neck of a bottle during aseptic procedures?
A: Yes, flaming the neck of a sterile bottle or flask is a crucial step in proper aseptic technique. The heat creates an upward convection current of sterile air, preventing airborne microorganisms from entering the container while it is open.
What is the key difference between aseptic and sterile?
The key difference is that sterile refers to a state of absolute freedom from all microorganisms, while aseptic technique is the set of actions taken to maintain sterility and prevent new contamination from occurring.