The field of medical device design is fundamentally a discipline of material science. Every component, from a temporary catheter to a permanent orthopedic implant, must interact with the complex biological environment of the human body in a predictable and safe manner. Without materials that can perform this function, the incredible advancements in surgical techniques, diagnostics, and patient care would not be possible. The selection and validation of biocompatible materials are therefore paramount to the success and safety of any medical product. These materials are not inert; rather, their interaction with host tissues determines the body’s response. A proper understanding of this dynamic relationship is a critical competency for any laboratory professional working in the biomedical field. This article explores the core principles, classifications, and testing methodologies for medical device materials, highlighting the essential role they play in modern healthcare.
The Science of Biocompatible Materials and Tissue Compatibility
At its heart, biocompatibility is the ability of a material to perform its intended function in a medical application with an appropriate host response. This "appropriate response" is often defined by the absence of toxicity, inflammation, or rejection. A truly biocompatible material does not simply exist passively within the body; it actively supports its function without causing harm. The concept can be broken down into three key responses: local, systemic, and functional. The local response relates to the material's interaction at the site of implantation, such as fibrous capsule formation around an implant. The systemic response involves the body's overall reaction, including immune and inflammatory system activation. The functional response is about whether the material maintains its mechanical and chemical integrity to perform its duty.
Achieving tissue compatibility is not just about avoiding a negative reaction. In many cases, it is about encouraging a positive one, such as the growth of bone onto an orthopedic implant. This is known as osseointegration. The surface chemistry and morphology of the material are critical determinants of this behavior. Proteins and cells interact with the material’s surface on a microscopic level, and this initial interaction dictates the long-term biological response. The material's surface energy, wettability, and roughness can all be engineered to promote specific cellular adhesion and proliferation, guiding the body’s healing process. The understanding of these intricate interactions is a primary focus of modern biomedical engineering.
A Guide to Medical Device Materials
The spectrum of medical device materials is broad, encompassing metals, polymers, and ceramics, each with unique properties that make them suitable for specific applications. The choice of material is a critical design decision, balancing mechanical strength, manufacturability, and biological response.
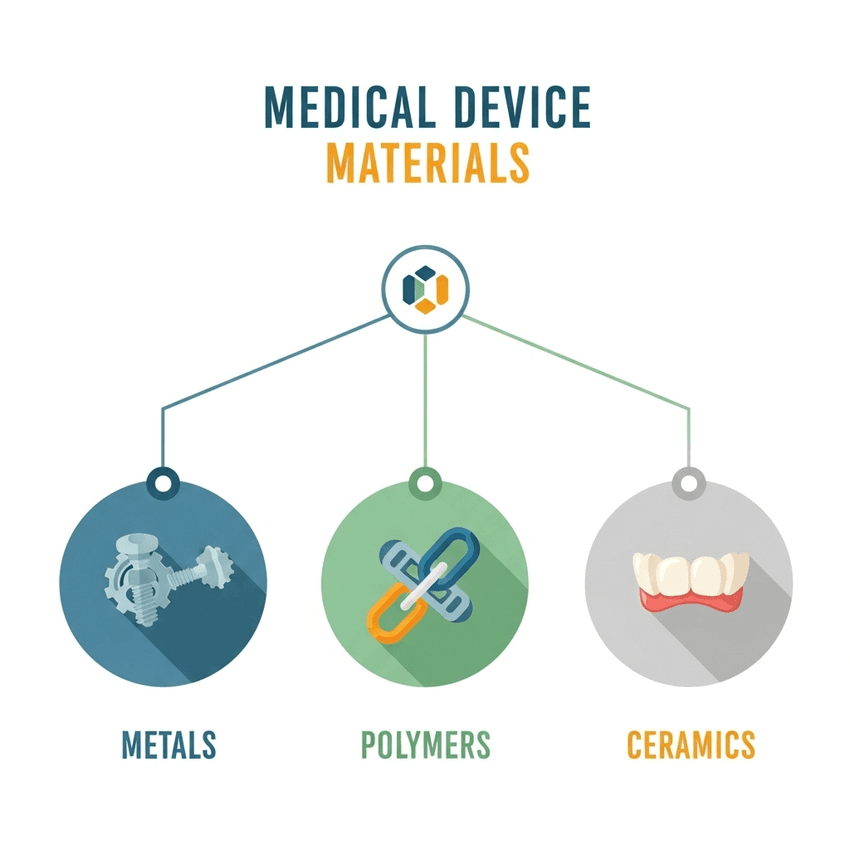
There are several options for medical device materials, each with their own benefits.
GEMINI (2025)
- Metals: Metals are valued for their high strength, durability, and fatigue resistance, making them ideal for structural applications.
- Titanium and Titanium Alloys: Widely used for bone implant materials, dental implants, and pacemakers. Known for excellent biocompatibility and osseointegration.
- Stainless Steel (316L): Common for surgical instruments, temporary implants (bone plates and screws), and stents due to its corrosion resistance and affordability.
- Cobalt-Chromium Alloys: Used for orthopedic implants and joint replacements where high strength and wear resistance are required.
- Polymers: Polymers are versatile, offering flexibility, lightweight properties, and tailored mechanical characteristics.
- Polyethylene (PE): Found in hip and knee joint components, acting as a low-friction bearing surface.
- Poly(tetrafluoroethylene) (PTFE): Used for vascular grafts due to its smooth surface and low thrombogenicity.
- Silicones: Widely used for catheters, tubing, and breast implants due to their flexibility and stability.
- Ceramics: Ceramics are known for their hardness, wear resistance, and high compressive strength.
- Alumina (Al2O3) and Zirconia (ZrO2): Used for dental crowns, hip joint balls, and femoral heads due to their exceptional hardness and wear properties.
- Calcium Phosphates: Valued for their similarity to bone mineral; used as coatings for metal implants to promote osseointegration.
Each of these material classes has a specific role in biomedical engineering, and the ongoing innovation in this field is driven by the development of novel materials and composite systems that combine the best properties of each.
Advancements in Implant Materials and Biomedical Engineering
The evolution of implant materials is a dynamic field driven by a desire for better patient outcomes, including longer implant lifespan, reduced complications, and improved tissue compatibility. A major focus has been on moving beyond passive materials to those that are bioactive and can actively participate in the healing process.
Bioactive materials, such as certain calcium phosphate ceramics, are designed to encourage a specific biological response, such as bonding with surrounding bone tissue. This approach minimizes the risk of implant loosening and provides a more durable solution. Another significant advancement is the use of porous or scaffold-like structures. These designs, often produced using advanced manufacturing techniques like 3D printing, mimic the natural porosity of bone, allowing for ingrowth of bone tissue and blood vessels. This enhances stability and integration, blurring the line between material and biological tissue.
Surface modification is a key strategy for improving existing biocompatible materials. Thin-film coatings, often applied using vapor deposition techniques, can alter the surface properties of an implant without changing its bulk characteristics. For example, a titanium implant can be coated with a thin layer of calcium phosphate to encourage rapid osseointegration. Drug-eluting coatings are also a notable advancement, where the surface releases a therapeutic agent (e.g., an antibiotic or anti-inflammatory drug) directly at the implant site, preventing infection and reducing inflammation. These techniques represent a powerful new tool in the biomedical engineering arsenal.
Rigorous Testing of Biocompatible Materials
The journey of medical device materials from the lab to clinical use is governed by a series of stringent regulations and standardized testing protocols. For the laboratory professional, understanding these requirements is non-negotiable. Regulatory bodies like the FDA and organizations like the International Organization for Standardization (ISO) provide clear guidelines for assessing biocompatibility.
The ISO 10993 series is the gold standard for biological evaluation. It outlines a systematic approach that includes a battery of tests to assess a material's biological effects.
- Cytotoxicity Testing: In vitro tests that determine if a material or its extracts are toxic to cells.
- Sensitization and Irritation Tests: In vivo tests that assess a material’s potential to cause allergic reactions or local irritation.
- Systemic Toxicity Tests: Evaluations to ensure the material does not release substances that cause adverse effects in organs or systems away from the implant site.
- Genotoxicity and Carcinogenicity Tests: Long-term studies to ensure the material does not induce genetic mutations or cancer.
In addition to biological testing, materials undergo rigorous mechanical and chemical characterization. Testing for corrosion resistance, wear rate, and fatigue strength is crucial for ensuring the long-term integrity and performance of the device. The meticulous process of documentation and validation is as important as the material selection itself, as it provides the evidence required for regulatory approval and ensures patient safety.
The Future of Biocompatible Materials in Biomedical Engineering
The demand for innovative and more effective medical devices will continue to drive advancements in biocompatible materials. The shift from materials that are simply tolerated by the body to those that actively engage with and promote biological function is transforming patient care. From bioresorbable scaffolds that dissolve as the body heals to materials that integrate seamlessly with living tissue, the future holds immense promise. For the laboratory professional, staying at the forefront of this field requires not only an understanding of material science but also a deep appreciation for the biological context in which these materials perform. The ongoing collaboration between material scientists, engineers, and clinicians is forging a new era of medical technology, grounded in the principles of safety, efficacy, and tissue compatibility.
Frequently Asked Questions About Biocompatible Materials
What is the primary difference between a biomaterial and a biocompatible material?
A biomaterial is a substance engineered to interact with biological systems for a medical purpose. A material becomes "biocompatible" if it is proven to be non-toxic and to elicit an appropriate host response for its intended application.
Why is titanium a common implant material?
Titanium is widely used as an implant materials due to its excellent combination of high strength, low density, and exceptional corrosion resistance. Most importantly, it is highly biocompatible and promotes osseointegration, allowing for a strong bond with bone tissue.
How does surface roughness affect tissue compatibility?
Surface roughness is a critical factor in tissue compatibility. A material with a certain level of roughness can promote cell adhesion and ingrowth, such as in the case of bone integration, whereas an ultra-smooth surface may be necessary to minimize platelet adhesion and prevent blood clot formation.
What are the key ISO standards for testing biocompatible materials?
The ISO 10993 series is the primary set of standards for biological evaluation of medical device materials. It covers a range of tests including cytotoxicity, sensitization, irritation, and systemic toxicity, among others.