The modern healthcare ecosystem relies fundamentally upon the accuracy and efficiency of clinical labs and medical labs. These essential departments serve as the diagnostic backbone for patient management, shifting the focus from simply generating results to providing clinically actionable insights that directly influence therapeutic decisions and population health strategies. The contemporary clinical lab environment is defined by its increasing complexity, driven by advancements in genomic testing, the necessity for decentralized testing models, and persistent pressures for stringent cost control. Successfully navigating this landscape requires laboratory professionals to maintain impeccable quality standards and manage intricate logistical networks. Continuous integration of emerging technologies is essential to preserve the integrity of the diagnostic process from specimen collection through final result interpretation.
Optimizing multisite clinical diagnostics and operational scale
Managing distributed laboratory operations across multiple locations, or multisite clinical diagnostics, presents unique management challenges that require robust standardization and technological integration. The proliferation of point-of-care testing (POCT) and regional draw sites necessitates centralized control over these decentralized activities. This ensures uniformity in quality management systems (QMS). Operational efficiency in this model hinges on the seamless flow of data, specimens, and quality metrics across the entire enterprise. Achieving this integration is paramount for large reference medical labs where economies of scale are vital for competitive advantage.
Strategies for standardization and cost control
Effective cost control is not achieved through simple budget cuts but through strategic optimization of workflows and resource utilization across all sites. Standardization of reagents, consumables, and instrumentation profiles across all linked clinical labs mitigates inventory complexity and allows for stronger vendor negotiation power. Furthermore, utilizing advanced logistics management systems ensures specimens are processed rapidly, minimizing the risk of degradation and the subsequent need for costly recollects or repeat testing.
Key elements for optimizing multisite operations include:
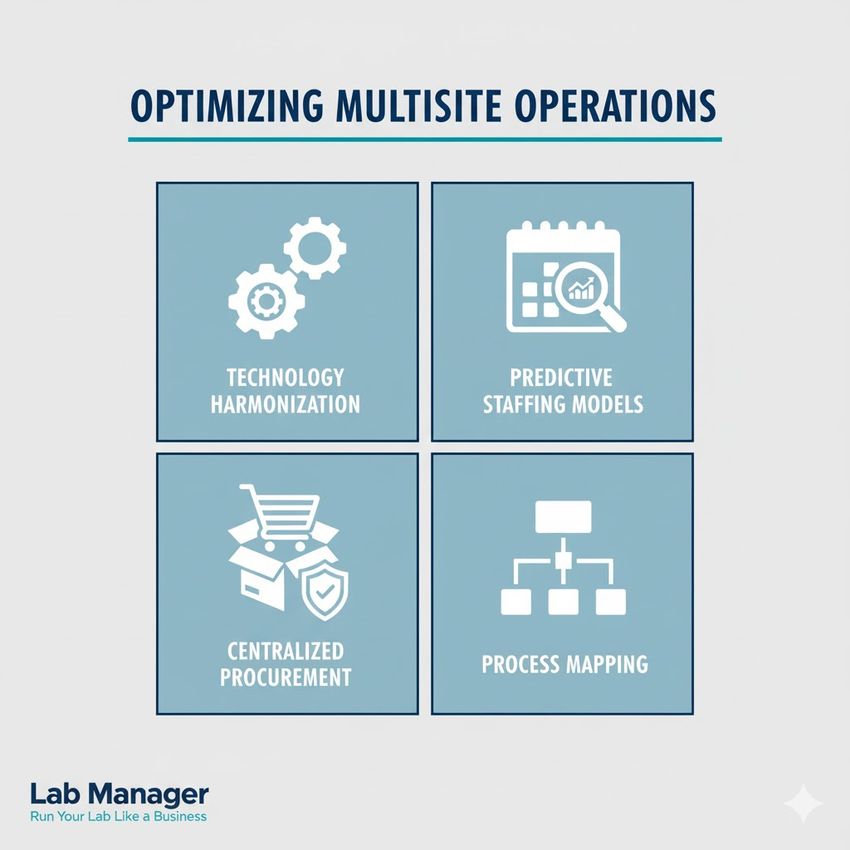
Optimize, standardize, succeed. Elevate your multisite strategy with these key areas of focus.
GEMINI (2025)
- Technology harmonization: Implementing a unified Laboratory Information Management System (LIMS) across all sites to enforce standardized test menus, reference ranges, and result formatting. This eliminates data silos and supports consistent clinical decision support.
- Predictive staffing models: Employing analytics to forecast testing volume fluctuations by site and shift. This permits dynamic staffing adjustments, ensuring adequate coverage without the excessive overhead of over-staffing, contributing significantly to cost control.
- Centralized procurement: Consolidating purchasing decisions for high-volume reagents and capital equipment. Volume purchasing significantly lowers the unit cost, directly addressing the pressure points associated with laboratory operational expenses.
- Process mapping: Developing comprehensive, identical standard operating procedures (SOPs) for non-analytic tasks (e.g., specimen accessioning, documentation, quality assurance checks) that are enforced uniformly across all locations involved in multisite clinical diagnostics.
Ensuring sample integrity and pre-analytic quality
The pre-analytic phase—which encompasses specimen collection, handling, transport, and preparation—remains the most frequent source of error in laboratory medicine. This phase directly impacts diagnostic reliability. Maintaining sample integrity is a critical, foundational quality measure for all medical labs. The quality of the final result, regardless of the sophistication of the analytic platform, is fundamentally dependent on the quality of the sample received. Errors introduced during the pre-analytic phase are often irreversible and can lead to misleading results. This potentially causes inappropriate patient treatment or delayed diagnosis.
Critical control points for pre-analytic excellence
To safeguard sample integrity, laboratory procedures must meticulously govern time, temperature, and volume variables. For molecular diagnostics and specialized chemistries, timely processing is essential to prevent degradation of nucleic acids or analytes. Temperature control is particularly crucial for heat-labile samples. Implementing real-time temperature monitoring for transport containers and storage units is a necessary preventative measure, consistent with guidelines provided in documents like the Clinical and Laboratory Standards Institute's (CLSI) PRE04.
Pre-analytic Variable | Potential Diagnostic Impact | Mitigation Strategy |
|---|---|---|
Volume (QNS) | Inability to run reflex or confirmatory testing, delayed results. | Automated draw systems that verify minimum fill volumes; training refresher programs. |
Hemolysis/Lipemia | Interferences leading to false increases or decreases in analyte concentration. | Standardization of phlebotomy technique; clear rejection criteria and communication. |
Temperature Excursion | Analyte degradation (e.g., coagulation factors, hormones) or cell viability loss. | Validated cold chain logistics; temperature loggers for long-distance transport. |
Misidentification | Catastrophic patient safety incident and misdiagnosis. | Double-labeling checks at the bedside/draw station; positive patient identification systems. |
Continuous education and competency assessment of all personnel involved in specimen acquisition, including phlebotomists and nursing staff, are critical investments that uphold the quality reputation of clinical labs.
Implementing advanced biosafety and compliance frameworks
The regulatory landscape governing clinical labs and medical labs is multilayered, requiring adherence to both mandatory federal regulations and often voluntary, but high-value, international standards. The commitment to biosafety and comprehensive regulatory compliance is non-negotiable, protecting laboratory personnel, the community, and the integrity of the diagnostic output.
Navigating CLIA and ISO standards
In the United States, the Clinical Laboratory Improvement Amendments (CLIA) establishes mandatory quality standards for all testing performed on human specimens for diagnosis, prevention, or treatment of disease. CLIA compliance is administered by the Centers for Medicare & Medicaid Services (CMS). It focuses heavily on personnel qualifications, quality control, proficiency testing, and facility standards based on test complexity (waived, moderate, or high). Recent revisions to CLIA personnel requirements, effective in late 2024, emphasize enhanced educational criteria and mandatory continuing education for key roles, signaling a rising bar for expertise in the clinical lab setting.
In contrast, the International Organization for Standardization (ISO) 15189 standard specifically addresses quality and competence for medical labs. While ISO 15189 accreditation is voluntary, it provides a globally recognized framework emphasizing continual improvement, risk management, and quality management system (QMS) integration that often surpasses minimum regulatory requirements. Adherence to CLIA and ISO standards provides a robust, dual-layered quality assurance structure.
Biosafety levels and risk management
Maintaining stringent biosafety protocols is essential in clinical labs handling potentially infectious material. Risk assessment informs the designation of Biosafety Levels (BSLs), which dictate containment practices, equipment, and facility design.
- Administrative controls: Establishment of written safety manuals, continuous training, medical surveillance programs, and emergency response plans.
- Engineering controls: Implementation of biological safety cabinets (BSCs), validated ventilation systems, eye wash stations, and secured access controls.
- Work practice controls: Strict adherence to personal protective equipment (PPE) requirements, aseptic techniques, sharps disposal policies, and decontamination procedures.
The prompt management of biohazards, including exposure protocols and waste disposal (as governed by OSHA regulations), ensures a safe working environment and prevents contamination that could compromise diagnostic accuracy.
Strategic selection and integration of diagnostic platforms
The choice and deployment of diagnostic platforms represent a critical capital and operational decision for modern medical labs. The transition from manual methods to highly automated, integrated systems directly influences turnaround time, throughput capacity, and overall cost control. The optimal selection process must move beyond simple assay performance metrics to consider total operational cost, interoperability, and long-term scalability.
Evaluation criteria for technology adoption
When considering new diagnostic platforms—whether for chemistry, hematology, microbiology, or molecular testing—laboratory leadership evaluates several factors to maximize return on investment and clinical utility:
- Throughput and batching: Assessing the system's ability to handle peak volumes and determining the optimal batch size versus continuous random access capabilities.
- Interoperability: The ease with which the instrument connects bidirectionally with the LIMS. Platforms with poor middleware or LIS connectivity can undermine efficiency gains and increase transcription error risks.
- Automation potential: Evaluating pre- and post-analytic automation features, such as automated decapping, aliquoting, and archiving. High levels of automation are essential for maximizing personnel efficiency and enabling better cost control.
- Reagent management and stability: Analyzing the complexity of onboard stability, calibration frequency, and the proprietary nature of reagents, which often have significant long-term cost control implications.
- Test menu breadth: Platforms offering a broad, integrated test menu can reduce the number of separate instruments required, simplifying training and maintenance.
Strategic integration often involves modular automation systems that link multiple diagnostic platforms across different specialties. These systems allow for continuous processing and dynamic sample routing, significantly reducing manual handling steps and optimizing resource allocation across clinical labs.
Designing patient-centered labs and enhancing clinical impact
The concept of designing patient-centered labs emphasizes a shift in focus from inward-looking operational metrics (e.g., machine utilization) to external clinical value delivery (e.g., impact on diagnosis and treatment efficacy). This patient-centric approach fundamentally redefines the role of the laboratory as an active, consultative partner in patient care, moving beyond mere testing services.
The role of the laboratory in clinical decision support
A key component of enhancing patient impact is the effective communication of results and participation in clinical consultation. The lab report should be designed not just as a statement of analytical fact, but as a tool for clinical interpretation. This includes:
- Critical value management: Implementing robust, validated protocols for reporting critical results immediately, ensuring direct communication between laboratory personnel and the responsible healthcare provider.
- Interpretive reporting: Providing interpretive comments, especially for complex or esoteric testing (e.g., genetic sequencing, tumor markers), which synthesize results and place them within the clinical context.
- Clinical consultation: Making highly qualified technical supervisors and pathologists accessible for consultation, helping clinicians select the correct test, interpret complex findings, and understand the limitations of assays.
By embracing the principles of designing patient-centered labs, medical labs directly influence the speed and accuracy of diagnosis, contributing measurable value to patient outcomes. This extends to transparency in turnaround times (TATs) and ensuring that the entire laboratory process, including phlebotomy services and result delivery, minimizes patient anxiety and maximizes clinical utility.
Driving excellence and strategic value in clinical diagnostics
The trajectory of the modern clinical lab is defined by dynamic technological change and persistent regulatory evolution. Laboratory professionals are tasked with simultaneously managing complex quality assurance programs while strategically implementing diagnostic platforms and optimizing multi-site logistics. The pursuit of operational excellence, underpinned by strict adherence to CLIA and ISO standards, is not merely a bureaucratic requirement but a fundamental imperative for ensuring public health and patient safety. Sustained success for medical labs requires a proactive approach to technology integration, continuous investment in personnel competency, and an unwavering focus on maintaining sample integrity across all operations. By embracing these principles, laboratory leaders ensure the clinical lab remains the indispensable source of data driving effective clinical practice and substantial patient impact.
Frequently asked questions (FAQ)
How do CLIA and ISO 15189 differ in their application to clinical labs?
CLIA (Clinical Laboratory Improvement Amendments) constitutes the mandatory federal regulatory standard in the United States, applying to all clinical labs performing diagnostic testing on human specimens. Oversight is determined by test complexity (waived, moderate, or high), and compliance is necessary for legal operation and Medicare/Medicaid reimbursement. ISO 15189, on the other hand, is a voluntary international standard specifying requirements for quality and competence in medical labs. ISO 15189 offers a comprehensive framework for a Quality Management System (QMS) emphasizing continual improvement and risk mitigation, often exceeding CLIA’s baseline requirements. While CLIA ensures a minimum standard, seeking ISO 15189 accreditation demonstrates an elevated commitment to quality and is often valuable for multisite clinical diagnostics and international recognition.
What are the primary strategies for effective cost control without compromising quality?
Effective cost control in clinical labs relies on process engineering rather than simple expense reduction. Primary strategies include standardizing test methodologies and reagents across all multisite clinical diagnostics locations to leverage volume purchasing and minimize inventory waste. Secondly, investing in automation and integrated diagnostic platforms reduces manual labor and minimizes consumables waste associated with manual processes. Finally, meticulous focus on pre-analytic quality, including ensuring sample integrity and reducing phlebotomy errors, avoids the hidden costs associated with repeat testing, delayed diagnosis, and subsequent downstream clinical expenses. Labor is a major cost driver, and optimizing staff through workflow analysis ensures maximum productivity.
How does biosafety compliance integrate with overall clinical lab quality management?
Biosafety compliance is an integral part of the overall Quality Management System (QMS) for medical labs. Regulations require stringent controls to protect laboratory personnel from infectious agents, preventing laboratory-acquired infections and accidental community release. This involves rigorous adherence to engineering controls (e.g., biological safety cabinets), administrative controls (e.g., exposure control plans), and work practice controls (e.g., universal precautions). Maintaining high biosafety standards ensures the physical safety of the environment, which in turn safeguards sample integrity by preventing cross-contamination of specimens. Compliance with CLIA and ISO standards mandates thorough documentation and continuous competency verification of these essential safety protocols.
In what way does designing patient-centered labs affect laboratory workflows?
Designing patient-centered labs shifts workflow priorities toward maximizing patient impact and clinical relevance. This perspective necessitates shorter, validated turnaround times (TATs) for critical tests and the adoption of interpretive reporting practices that aid clinical decision-making. Workflow adjustments include adopting lean and Six Sigma principles to remove non-value-added steps, optimizing pre-analytic processes to improve sample integrity, and enhancing communication channels to ensure timely delivery of results. Furthermore, the laboratory’s physical and technological design must support consultation and collaboration, positioning the clinical lab staff as active members of the patient care team rather than solely as service providers.
This article was created with the assistance of Generative AI and has undergone editorial review before publishing.