Microscopy in forensic pathology serves as a fundamental diagnostic tool used to confirm gross findings. It identifies microscopic pathologies that are invisible to the naked eye during a standard autopsy. By examining tissue sections at the cellular level, forensic pathologists can differentiate between natural disease processes and traumatic injuries with high precision. This scientific rigor is essential for establishing a definitive cause of death. It also provides objective evidence in medicolegal proceedings. Histological analysis often serves as a decisive tool in "negative autopsies" where no macroscopic cause of death is apparent. This ensures that subtle lethal conditions, such as cardiac conduction system defects or early-stage sepsis, are not overlooked by the medical examiner.
How does microscopy in forensic pathology assist in death investigation?
Microscopy in forensic pathology provides the definitive cellular evidence required to confirm or refute preliminary findings made during the gross examination of a body. This process involves the histological analysis of tissue samples, typically stained with hematoxylin and eosin (H&E), to identify specific pathological changes at the micron scale. Forensic practitioners rely on these microscopic observations to detect subtle signs of disease, poisoning, or injury. These findings are often not visible to the naked eye during the initial autopsy phase.
The use of microscopy allows for the identification of systemic infections and early-stage myocardial infarctions. It also identifies specific types of pulmonary edema that might be misclassified during a gross internal exam. According to the National Association of Medical Examiners (NAME), histological examination is a standard component of a complete autopsy. It is specifically used when the cause of death is not readily apparent from gross findings or when the circumstances of death are suspicious. By documenting these cellular changes, pathologists create a verifiable, permanent record. This record can be presented as objective evidence in criminal or civil court cases.
Microscopic evaluation is also vital for distinguishing between antemortem and postmortem injuries. This is a frequent challenge in medicolegal death investigation. Pathologists look for "vital reactions" within the tissue architecture, such as leucocyte infiltration, fibrin deposition, or hemorrhage. These markers indicate that the individual was alive when the injury occurred. This distinction is critical in cases involving suspected physical abuse, elder neglect, or foul play. The timing of trauma determines the legal trajectory and potential charges in an investigation.
Condition | Gross Finding | Microscopic Finding (Microscopy in Forensic Pathology) |
|---|---|---|
Early Myocardial Infarction | Normal or pale muscle | Contraction bands, wavy fibers, neutrophilic infiltrate |
Sepsis | Splenomegaly | Acute splenic tumor, neutrophilic sequestration |
Fat Embolism | Usually invisible | Fat globules in pulmonary capillaries (Oil Red O stain) |
What are the common histological stains used in forensic microscopy?
Standard and specialized histological stains are used in microscopy in forensic pathology to highlight specific cellular structures and pathogens. They also identify foreign substances within tissue samples. The primary stain used in virtually every forensic lab is hematoxylin and eosin (H&E). It provides a general overview of tissue morphology by staining nuclei blue/purple and cytoplasm various shades of pink. When standard H&E staining is insufficient to provide a definitive diagnosis, pathologists utilize "special stains." These stains identify specific pathogens, minerals, or chemical compounds associated with the death.
- Prussian Blue: This stain is used to detect hemosiderin, which is a byproduct of hemoglobin breakdown. Its presence indicates older hemorrhages or chronic iron overload.
- Masson’s Trichrome: This stain is effective for identifying collagen fibers. It helps pathologists assess the age of scars or fibrotic changes in the heart.
- Grocott-Gomori Methenamine Silver (GMS): This silver-based stain is utilized to visualize fungal organisms and certain bacteria. It is commonly used in suspected infection cases.
- Ziehl-Neelsen: This is the standard stain for identifying acid-fast bacilli. It is specifically used for Mycobacterium tuberculosis in pulmonary or systemic granulomas.
- Oil Red O: This stain is used on frozen sections to identify fat emboli in the lungs or brain. It typically follows long-bone fractures or soft tissue trauma.
The selection of these stains is guided by the clinical history and scene investigation. It is also informed by the gross findings observed during the autopsy. For instance, a Gram stain on lung tissue can confirm the presence of bacterial pneumonia. This might be a primary or contributing factor to respiratory failure. These methodologies follow established protocols set by organizations such as the College of American Pathologists (CAP). They ensure results are reproducible and accurate for legal scrutiny.
How is the timing of an injury determined using microscopy?
Microscopy in forensic pathology enables the estimation of injury age by observing the body's inflammatory and healing responses. The transition from acute inflammation to the formation of granulation tissue follows a predictable biological timeline. Pathologists analyze the presence of specific cell types, such as neutrophils, macrophages, and fibroblasts. These observations help narrow down the window of time in which an injury was sustained relative to the time of death.
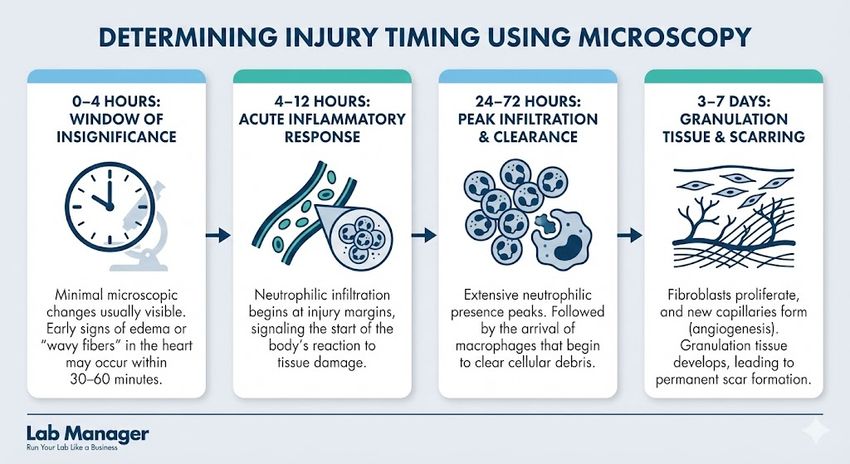
This infographic illustrates the timeline of microscopic changes that occur in injured tissue, helping pathologists determine the age of an injury.
GEMINI (2026)
- 0–4 hours: Minimal microscopic changes are usually visible in this "window of insignificance." Early signs of edema or "wavy fibers" in the heart may occur within 30–60 minutes.
- 4–12 hours: Neutrophilic infiltration begins at the margins of the injury. This signals the start of the acute inflammatory response as the body reacts to tissue damage.
- 24–72 hours: Extensive neutrophilic presence peaks during this period. It is typically followed by the arrival of macrophages that begin to clear cellular debris.
- 3–7 days: Fibroblasts begin to proliferate and new capillaries form through angiogenesis. This marks the development of granulation tissue, which eventually leads to a permanent scar.
While these timelines provide a useful framework, forensic professionals must account for individual variables. Factors such as the victim's age, underlying health status, and environmental conditions can alter the rate of healing. The precision offered by histological timing is often the deciding factor in reconstructing the events leading up to a death. It is particularly useful when trying to verify a witness's timeline.
What is the role of microscopy in identifying environmental and toxic exposures?
Microscopy in forensic pathology is a critical diagnostic method for detecting foreign particulates. It also identifies cellular changes associated with environmental toxins or illicit drug use. Pathologists use polarized light microscopy to identify birefringent materials. These are substances that refract light in two directions, such as talc, starch, or silica. These materials are often found in the lungs or injection sites of intravenous drug users. Microscopic evidence can link a specific substance directly to the physiological cause of death.
The detection of soot and thermal injury in the airways is a classic application of microscopy. It is used to determine if a fire victim was alive and breathing during the blaze. Microscopic examination of the lungs or trachea may reveal "smoke inhalation" markers. These include carbon-laden macrophages deep within the alveoli or epithelial necrosis in the bronchi. This helps investigators distinguish between a person who died before a fire was set and one who perished due to smoke inhalation.
In cases of heavy metal poisoning, microscopy can reveal characteristic inclusion bodies or patterns of organ damage. For example, chronic lead poisoning may manifest as acid-fast intranuclear inclusion bodies within the renal tubular cells. This finding is highly specific when correlated with toxicological data. These specific findings are essential for directed toxicological testing. They provide an evidence-based explanation of how environmental factors contributed to the decedent's demise.
Forensic microscopy in the identification of gunshot residue and tool marks
Microscopy in forensic pathology extends beyond traditional light microscopy to include the analysis of trace evidence. This includes gunshot residue (GSR) and tool marks on bone or skin. Scanning Electron Microscopy (SEM) combined with Energy Dispersive X-ray Spectroscopy (EDX) is the gold standard for this analysis. It allows forensic scientists to identify the unique spherical shape and elemental composition of GSR particles. This imaging is far more definitive than traditional chemical "color" tests for determining if a wound is an entrance point.
Scanning electron microscopy is specifically utilized to analyze the morphology of particles found on the hands or clothing. The ability to visualize these microscopic elements helps in reconstructing the distance and angle of a firearm discharge. This is often a point of contention in self-defense claims. This objective data is especially crucial when the physical evidence at the scene is ambiguous. It is also vital when decomposed remains are being examined and traditional skin markers are lost.
Beyond firearms, microscopy is used to examine "kerf" marks or strike patterns on skeletal remains. These are caused by sharp or blunt instruments like saws, knives, or hammers. By viewing these marks under magnification, a pathologist or forensic anthropologist can often determine the type of blade used. They can identify the number of teeth on a saw or the direction of the blow. These details provide investigators with a "fingerprint" of the weapon. This can be compared against tools found in a suspect's possession following established forensic anthropology guidelines.
Integrating digital pathology and artificial intelligence in forensic practice
Digital pathology represents the most significant modern advancement in microscopy in forensic pathology. It allows for the high-resolution scanning of physical glass slides into digital formats. This technology enables "virtual microscopy" where pathologists can view tissue sections on a computer monitor. They can apply digital measurements and use automated algorithms to quantify cellular features. The transition to digital formats facilitates rapid peer review and "telepathology" for global consultations.
Artificial intelligence (AI) and machine learning models are currently being developed to assist forensic pathologists. These models help in identifying subtle patterns that may be missed during manual screening. For example, AI algorithms can be trained to detect early signs of myocarditis. They can also quantify the ratio of different inflammatory cells to more accurately date an injury. These computational tools do not replace the pathologist. Instead, they act as a sophisticated "second pair of eyes" to increase objectivity.
The use of digital microscopy also improves the long-term storage and accessibility of forensic evidence. Physical slides can fade or break over decades. Digital images can be stored in secure, redundant databases for cold case reviews or future legal appeals. As forensic labs continue to modernize, the integration of digital imaging and AI will likely become the standard. This ensures the most robust scientific testimony possible in the courtroom.
Conclusion: The importance of microscopy in modern forensic practice
Microscopy in forensic pathology remains an indispensable pillar of death investigation. It provides the cellular context necessary for accurate and legally defensible diagnoses. By integrating traditional histological staining with advanced imaging techniques, pathologists can resolve complex questions. These include matters of injury timing, disease progression, and toxic exposure. The evidence generated through microscopic analysis is objective and reproducible. It provides the scientific foundation required for the medicolegal system to function effectively. As technology continues to evolve, computational pathology will further enhance the ability of medical examiners to provide clarity and justice.
This article was created with the assistance of Generative AI and has undergone editorial review before publishing.












