Particle characterization is a fundamental requirement for the safety and efficacy of inhalation therapies. These therapies are designed to treat both pulmonary and systemic conditions. The physiological constraints of the respiratory tract dictate specific particle size requirements. Only particles within a precise aerodynamic range can bypass the upper airways and reach the deep lung. Accurate particle characterization allows laboratory professionals to predict deposition patterns and stabilize formulations. It is also necessary to meet stringent regulatory requirements for Orally Inhaled and Nasal Drug Products (OINDPs).
Why is particle size critical for inhalation therapies?
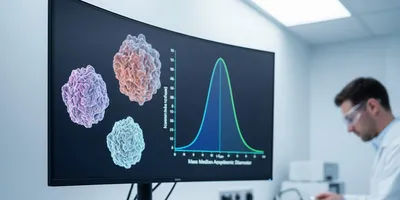
The effectiveness of inhalation therapies depends on achieving a Mass Median Aerodynamic Diameter (MMAD) typically between 1 micrometer and 5 micrometers to ensure deep lung penetration. Particles larger than 5 micrometers generally deposit in the oropharynx via inertial impaction. Conversely, particles smaller than 0.5 micrometers are often too light to settle and may be exhaled before they can provide therapeutic benefit.
Precise particle characterization ensures that the Fine Particle Fraction (FPF) remains consistent throughout the product’s shelf life. The FPF represents the portion of the dose likely to reach the lower respiratory tract. Maintaining this fraction is vital for the reproducibility of the delivered dose.
Laboratory professionals utilize laser diffraction and Cascade Impactors (CI) to determine these distributions. Laser diffraction provides rapid geometric size data, which is useful during early formulation stages. However, CIs measure aerodynamic behavior, which accounts for particle density and shape.
According to the United States Pharmacopeia (USP 601), aerodynamic assessment is the gold standard for characterizing the delivered dose. This applies to both metered-dose inhalers (MDIs) and dry powder inhalers (DPIs). These standards ensure that laboratory data correlates with expected clinical outcomes.
The deposition of particles in the respiratory tract is governed by three primary physical mechanisms. These are inertial impaction, gravitational sedimentation, and Brownian diffusion. Impaction occurs in the upper airways where air velocity is high and the airway path changes abruptly.
This mechanism primarily affects particles typically larger than 5 micrometers in diameter. Sedimentation is the dominant mechanism for particles sized 1 micrometer to 5 micrometers in the smaller airways. In these regions, the airflow velocity is much lower, allowing gravity to take effect.
Diffusion governs the movement of sub-micron particles (less than 0.5 micrometers) in the alveolar regions of the lungs. Understanding these mechanisms allows scientists to engineer particles that target specific zones. This targeting is the basis for modern localized pulmonary treatment strategies.
How does particle morphology influence drug delivery?
Particle morphology, including shape and surface roughness, significantly impacts the flowability and aerosolization efficiency of inhalation therapies. Non-spherical or elongated particles often exhibit different aerodynamic drag compared to spherical counterparts. These shapes can also lead to interlocking behaviors that cause inconsistent dosing.
Detailed particle characterization via Scanning Electron Microscopy (SEM) helps scientists visualize these structural attributes. This visualization is essential for optimizing formulation stability during manufacturing. It also helps in identifying potential issues with powder dispersion during patient use.
Surface area and rugosity also play roles in the cohesive and adhesive forces between drug particles and carrier molecules. High surface roughness can reduce the contact area between the active pharmaceutical ingredient (API) and the carrier. This reduction can make it easier for the API to detach during inhalation.
Research published in the Journal of Aerosol Science (Finlay et al.) indicates that controlling surface morphology is essential for reducing "clumping." Clumping in dry powder inhalers can significantly reduce the respirable fraction of the drug. By managing surface rugosity, formulators can improve the efficiency of dose delivery.
Morphologically Directed Raman Spectroscopy (MDRS) has emerged as a powerful tool for characterizing individual components in a blend. This technique combines automated image analysis with Raman spectroscopy to provide chemically specific size data. It allows laboratory professionals to differentiate between the API and the excipient accurately.
This differentiation ensures that the particle characterization data reflects the actual drug behavior. Without MDRS, it is difficult to determine if a size change is due to the drug or the carrier. This clarity is crucial for troubleshooting formulation failures in the laboratory.
Modern particle engineering often aims to create "crumpled" or "raisin-like" surfaces on drug particles. These specific morphologies are designed to maximize aerosolization by minimizing inter-particle contact. Characterizing these complex shapes requires high-resolution imaging and sophisticated mathematical modeling.
What analytical techniques are used for particle characterization?
The most common techniques for particle characterization in respiratory drug development include Next Generation Impaction (NGI) and laser diffraction. The NGI is a high-resolution cascade impactor that separates particles into size-dependent fractions. This separation provides a direct correlate to human lung deposition patterns.
For rapid screening during early-stage formulation, laser diffraction offers a non-destructive measurement method. Instruments such as the Malvern Panalytical Spraytec are designed specifically for aerosol characterization. These systems provide volume-based size distributions in real-time at high sampling frequencies.
For nanoparticle-based inhalation therapies, Dynamic Light Scattering (DLS) is employed to measure hydrodynamic diameter. This is particularly relevant for nebulizer solutions or lipid-based delivery systems. Sub-micron accuracy is required to ensure these systems remain stable in suspension.
The International Organization for Standardization (ISO 13320:2020) provides the framework for laser diffraction methods. This standard ensures data integrity and reproducibility across different laboratory environments. Following these guidelines is essential for international regulatory submissions.
The Andersen Cascade Impactor (ACI) is another widely used instrument in the pharmaceutical industry. It consists of eight stages that simulate different levels of the human respiratory system. While older than the NGI, it remains a staple for many legacy products and regulatory filings.
Both the NGI and ACI require precise flow rate control to yield accurate data. The cut-off diameter (D50) for each stage is highly dependent on the velocity of the air. Laboratory professionals must calibrate these systems regularly to maintain measurement precision.
Abbreviated Impactor Measurements (AIM) are also becoming more popular for routine quality control. AIM systems use fewer stages to simplify the testing process while maintaining data relevance. These systems are particularly useful for high-volume manufacturing environments where speed is critical.
How does particle characterization ensure regulatory compliance?
Particle characterization serves as a critical quality attribute (CQA) that must be strictly controlled for safety. Regulatory bodies such as the FDA and EMA require comprehensive data on the Aerodynamic Particle Size Distribution (APSD). This data proves that inhalation therapies are both safe and effective for the target population.
Regulators require this information to prove that generic versions of drugs are bioequivalent to reference listed drugs. Without rigorous characterization, manufacturers cannot guarantee that the dosage reaches the therapeutic window. Consistent data helps avoid the risk of sub-therapeutic dosing or toxic side effects.
Stability testing also relies on these measurements to detect phenomena such as Ostwald ripening. This process involves the growth of larger particles at the expense of smaller ones over time. Monitoring these changes is a requirement for establishing the shelf life of a product.
The FDA’s "Guidance for Industry: Nasal Spray and Inhalation Solution, Suspension, and Spray Drug Products" outlines specific testing requirements. It highlights the necessity of characterizing particle size to prevent adverse events. Consistent reporting of MMAD and Geometric Standard Deviation (GSD) is a prerequisite for any NDA.
Furthermore, the concept of "Q3 equivalence" (physicochemical equivalence) is essential for abbreviated new drug applications (ANDAs). This involves demonstrating that the generic product has the same particle size distribution and crystalline state. It ensures that the generic performs exactly like the innovator product in the patient's lungs.
Advanced particle characterization techniques such as X-ray Powder Diffraction (XRPD) are often used here. XRPD confirms that no polymorphic transitions have occurred during the manufacturing or storage process. This structural integrity is vital for maintaining the solubility and efficacy of the inhaled drug.
Product-Specific Guidances (PSGs) from the FDA often mandate specific APSD benchmarks. These benchmarks are determined through extensive laboratory testing and clinical trials. Adhering to these guidelines is the only way to ensure a smooth path to market approval.
Understanding the role of excipients in particle behavior
Excipients such as lactose monohydrate or leucine are frequently added to inhalation therapies to act as carriers. These additives are characterized to ensure they provide the necessary surface energy to hold the drug. They must release the drug efficiently upon inhalation by the patient.
Particle characterization of the blend ensures that the drug-to-carrier ratio remains uniform. This uniformity prevents "dose dumping" where a patient receives too much drug at once. It also prevents inadequate delivery caused by drug particles staying stuck to the carrier.
Modern formulations often utilize "engineered particles" created through spray-drying. These particles are often low-density, porous spheres that behave like much smaller particles in the air. Characterizing the porosity and density of these systems is vital for predicting their flight path.
The interaction between the API and the carrier is often quantified using the Fine Particle Mass (FPM). This represents the actual mass of the drug that is small enough to be respirable. Laboratory professionals must ensure that the carrier particles are large enough to be captured in the mouth.
Typically, carrier particles are larger than 40 micrometers to ensure they do not reach the lungs. This requires a dual-track approach to particle characterization in the laboratory. One must analyze both the fine drug fraction and the coarse carrier fraction simultaneously.
Surface energy measurements, such as Inverse Gas Chromatography (IGC), are also used to study these interactions. IGC helps scientists understand the strength of the bond between the drug and the excipient. This understanding is key to designing formulations that disperse easily during inhalation.
Environmental impact on particle stability and measurement
Environmental conditions, particularly relative humidity (RH), significantly alter the results of particle characterization. High humidity can lead to moisture uptake in hygroscopic powders, causing particles to stick together. This agglomeration leads to a subsequent increase in the measured MMAD.
To ensure data accuracy, laboratory professionals must perform characterization in climate-controlled environments. These environments should mimic both the storage conditions and the conditions within the human lung. Controlling RH is one of the most challenging aspects of aerosol science.
Moisture can also induce phase transitions in amorphous drug particles, leading to crystallization. These changes directly affect the aerosolization efficiency and the Fine Particle Fraction. Research in Advanced Drug Delivery Reviews emphasizes the importance of moisture-dependent characterization.
Standardized testing protocols often require pre-conditioning of the powder at specific humidity levels. Dry powder inhalers are particularly sensitive to static electricity and moisture during the testing process. These factors can influence the "plume" geometry and the speed of the aerosol cloud.
Integrating environmental sensors into particle characterization workflows allows for more robust data sets. This data reflects real-world patient usage scenarios more accurately than testing in a vacuum. It helps manufacturers design better packaging to protect the drug from environmental degradation.
As global temperatures and humidity levels fluctuate, this area of research becomes increasingly important. Scientists are now investigating how "extreme" environments affect the delivery of life-saving medications. This work ensures that inhalation therapies remain effective in all geographic regions.
Conclusion: the future of particle characterization in respiratory medicine
Advanced particle characterization remains the cornerstone of successful drug delivery for all inhalation therapies. By integrating aerodynamic measurements with morphological analysis, laboratory professionals can develop more effective treatments. The continued evolution of high-resolution imaging and real-time sensing will further refine our ability to target the lungs.
Future developments are likely to focus on in vitro-in vivo correlation (IVIVC). This involves using laboratory-based particle characterization data to predict clinical outcomes in patients. As personalized medicine advances, we may see therapies tailored to an individual’s specific airway geometry.
The precision of our analytical tools dictates the safety and reliability of the medications delivered to millions. Particle characterization will continue to drive innovation in the pharmaceutical industry for decades to come. Ultimately, this scientific rigor ensures that every breath a patient takes delivers the intended therapeutic effect.
This article was created with the assistance of Generative AI and has undergone editorial review before publishing.