Cell & Tissue Culture

A new study led by researchers at The Scripps Research Institute (TSRI) and the University of California (UC), San Diego School of Medicine shows that certain stem cell culture methods are associated with increased DNA mutations. The study points researchers toward safer and more robust methods of growing stem cells to treat disease and injury.

Researchers at the University of California, Davis, will explore ways to speed production of the Ebola drug Zmapp with a $200,000 rapid-response grant from the National Science Foundation.

Problem: Scientists must typically rely on high-end cell sorters in core facilities to run their samples. These cell sorters—equipped with five or more lasers and double digit detection channels—were originally utilized to answer pressing questions arising in the immunology field. However, they are overly complex for the new breed of user who sorts cells today: cell biologists and biochemists who employ fluorescent proteins and require at most four colors and one-to-two population sorting. The challenge is that as demand increases, the number of staff available to operate these complex instruments remains the same. As a result, wait times at core facilities have ballooned, literally putting research on hold until capacity is available. For the more than half of today’s cell sorting users who require four colors or
fewer sorts, the elaborate equipment is becoming a bottleneck.

A novel jelly-like substance developed by Kansas State University researchers was recently issued a U.S. patent. The substance may be used for biomedical applications, ranging from cell culture and drug delivery to repairing and replacing tissue, organs and cartilage.
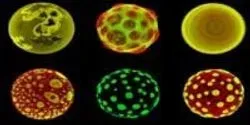
How did life originate? And can scientists create life? These questions not only occupy the minds of scientists interested in the origin of life, but also researchers working with technology of the future. If we can create artificial living systems, we may not only understand the origin of life - we can also revolutionize the future of technology.

Geoffrey Bartholomeusz, PhD, associate professor in the Department of Experimental Therapeutics and director of the siRNA Core Facility at the University of Texas MD Anderson Cancer Center, talks to contributing editor Tanuja Koppal, PhD, about why there is a growing interest in replacing some 2D cell culture applications with 3D cell cultures. He talks about where and why he uses 3D-based cell cultures in his lab and what lab managers should take into consideration before making the investment in this innovative technology.

For years, researchers and patients have hoped that embryonic stem cells (ESCs)—capable of forming nearly any cell type in the body—could provide insight into numerous diseases perhaps even be used to treat them. Yet progress has been hampered by the inability to transfer research and tools from mouse ESC studies to their human counterparts, in part because human ESCs are “primed” and slightly less plastic than the mouse cells.












